A
strong significant (p = .001) negative correlation was found between TBUT and
minus power of contact lens (Table 2). Regression model shows that with -1 D increase in power
of contact lens, TBUT decreased by -.263
times (Figure 3).
No significant (p
> 0.05) association was found between corneal changes and plus power of
contact lens.
DISSCUSSION
In this study a
decreased value of TBUT was found in majority of contact lens users. The results determined that 67% of contact lens users had
abnormal TBUT. The reason might be that the
contact lens induced hypoxia interfered with tear film stability and resulted
in shortened TBUT. These results were similar to the studies of Sweeney et al.1, Craig et al.3, Eghosasere et al.4, Du Toitet al.6, Thai et al.7, Glasson et al.8, Nichols and Sinnot9,
Riley et al.10, Stapleton et al.[11], Janine
et al.12, Guillon and
Maissa13, Jansen et al.14,
Shrestha et al.15, Young et al.16, Kastelanet al.17, Gupta et al.18
and Pili et al.19. However
these findings were contrary to the results reported by Santodomingo-Rubido et al.20 study. This could be
due to the regional, racial or environmental differences.
In this study no
significant association was found between TBUT and type of contact lens. The study results were similar to Craig et al.3 and Thai et al.7 studies. But contrary
to Sweeney et al.1,
Eghosasere
et al.4, Riley et al.10, Kastelan et al.17 studies which found association between TBUT and type of
contact lenses. The reason might be that more than half of total subjects used
soft contact lenses and proportions of other types of contact lens users were
less, therefore, could not find any significant association.
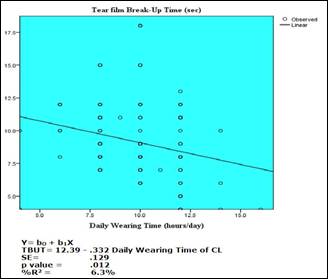
Fig. 1: Regression model of TBUT and daily wearing time of contact
lenses (showed that as the daily wearing time of contact lens increased, the
TBUT value decreased).
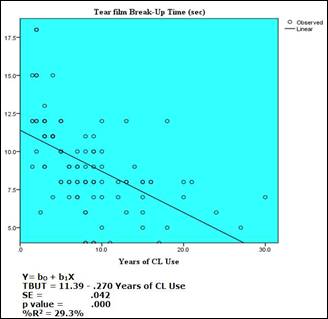
Fig. 2: Regression model of TBUT and Years of Contact Lens Use (showed
that as the number of years of contact lens use increased, the TBUT value
decreased).
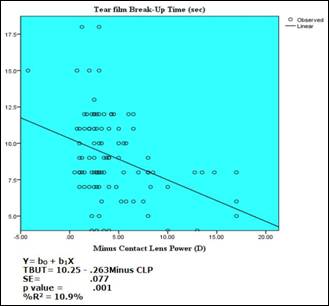
Fig. 3: Regression model of TBUT and
minus power of contact lenses (showed that as the minus power of contact lens
increased, the TBUT value decreased)
In
this study a significant negative correlation was found between TBUT and daily
wearing time of contact lenses. The reason could be that increased daily
wearing time of contact lens caused more hypoxia which adversely affected the
tear film stability. These results were in line with those reported by Kastelan
et al.17 study.
In
this study a highly significant negative correlation was found between TBUT and
years of contact lens use. This might be due to the reason that prolonged use
of contact lenses resulted in chronic hypoxia which unfavorably affected the
tear film stability. No other study could be found to sufficiently discuss the
results.
In
this study a strong significant negative correlation was found between TBUT and
minus power of contact lens. The reason could be that high power contact lenses
were thicker which reduced oxygen permeability and caused hypoxia which lead to
reduce TBUT. No other study was found to sufficiently discuss the results.
In this study no
significant association was found between corneal changes and plus power of
contact lens. These insignificant results could be due to very less number of
hyperopic contact lens users in the study. No other study was found to sufficiently
discuss the results.
CONCLUSION
It is concluded
that long term use of contact lenses decreased the stability of tear film and
thus TBUT. TBUT was more affected with increase in daily wearing time, years of
contact lens use and high minus power of contact lens.
Author’s Affiliation
Dr. Rabia Ammer
BSc Optom, Mphil
Optom.
Department of
Allied Health Sciences/ School of Optometry/ The University of Faisalabad.
Role of Authors
Dr. Rabia Ammer
Concept, Design of
study, Sample selection. Data collection, Data entry, Data analysis, Critical
review, Drafting and revision of manuscript.
REFERENCES
1.
Sweeney
D, Millar T, Raju S. Tear film
stability: A review. Experimental Eye Research, 2013; 117: 28-38.
2.
Williams L.
Anatomy and physiology of the anterior segment. Module1. Anterior segment of
the eye. The IACLE contact lens course. The International Association of
Contact Lens Educators Sydney, Australia, 2000; 1 (1): 3-80.
3.
Craig PJ, Willcox DPM, Arg¨ueso P, Maissa C, Stahl U, Tomlinson A,
Wang J, Yokoi N, Stapleton F. The
TFOS International Workshop on Contact Lens Discomfort: Report of the Contact
Lens Interactions with the Tear Film Subcommittee. Invest Ophthalmol Vis Sci. 2013; 54 (11): TFOS123.
4.
Eghosasere I, Joy EI, Joy OI. Effect of soft contact lens materials on tear film stability and
central corneal radius of curvature: A comparative study of Polymacon and
Lotrafilcon B. Sierra
Leone J Biomed Res. 2011; 3 (3): 144-150.
5.
Terry R.
Corneal oxygen requirements and the effects of hypoxia. Module 6. The cornea in
contact lens wear. The IACLE contact lens course. The International Association
of Contact Lens Educators Sydney, Australia, 2000; 1 (1): 3-36.
6.
Du Toit R, Situ P, Simpson T, Fonn D. The effects of six months of contact lens wear on the tear film,
ocular surfaces, and symptoms of presbyopes. Optom Vis Sci. 2001; 78 (6): 455-462.
7.
Thai
L, Tomlinson A, DoaneM. Effect of
Contact Lens Materials on Tear Physiology. Optom Vis
Sci. 2004; 81 (3): 194-204.
8.
Glasson M, Stapleton F, Willcox, M. Changes to tear film parameters during wear of HEMA-based hydrogel
lenses. Ocul Surf. 2005; 3 (1): 66.
9.
Nichols JJ, Sinnott TL. Tear film, contact lens, and patient-related factors associated
with contact lens–related dry eye. Invest Ophthalmol Vis Sci. 2006; 47 (4): 1319-1328.
10.
Riley C, Young G, Chalmers R. Prevalence of Ocular Surface Symptoms, Signs, and
Uncomfortable Hours of Wear in Contact Lens Wearers: The Effect of Refitting
with Daily-Wear Silicone Hydrogel Lenses (Senofilcon A). Eye Contact Lens, 2006; 32 (6): 281-286.
11.
Stapleton F, Stretton S, Papas E, Skotnitsky C, Sweeney DF. Silicone hydrogel contact lenses and the ocular surface. Ocul
Surf. 2006; 4 (1): 24-43.
12.
Janine A, Smith AJ, Albeitz J, Begley C, Caffery B, Nichols K,
Schaumberg D, Schein O. The
epidemiology of dry eye disease: report of the epidemiology subcommittee of the
international dry eye work shop. Ocul Surf. 2007; 5 (2): 93-107.
13.
Guillon M, Maissa C.
Contact lens wear affects tear film evaporation. Eye Contact Lens, 2008; 34 (6):
326-330.
14.
Jansen M, Begley C, Himebaugh N, Port N. Effect of contact lens wear and a near task on tear film break-up.
Optom Vis Sci. 2010; 87 (5): 350-357.
15.
Shrestha G, Sujakhu D, Shrestha JB, Shrestha JK. Tear film evaluation in contact lens wearers and non wearers. Journal of Institute of Medicine,
2012; 34 (2): 14-20.
16.
Young G, Chalmers R, Napier L, Kern J, Hunt C, Dumbleton K. Soft contact lens-related dryness with and without clinical
signs. Optom Vis Sci. 2012; 89 (8): 1125-1132.
17.
Kastelan
S, Lukenda A, Salopek-Rabatic J, Pavan J, Gotovac M.
Dry eye symptoms and signs in long-term contact lens wearers. Coll Antropol.
2013; (37) 1: 199–203.
18.
Gupta A, Shah M, Samanta A. Effect of extrinsic controls on blinking and tear film stability
among soft contact lens wearers. International
Journal of Medicine & Health Research, 2014; 1 (1): 1-7.
19.
Pili K, Kaštelan S, Karabatic M, Kasun B, Culig B. Dry eye in contact lens wearers as a growing public health
problem. Psychiat Danub. 2014; 26 (3): 528-532.
20.
Santodomingo-Rubido J, Wolffsohn JS, Gilmartin B. Changes in ocular physiology, tear film characteristics, and
symptomatology with 18 months silicone hydrogel contact lens wear. Optom Vis
Sci. 2006; 83 (2): 73-81.